Alcohol withdrawal symptoms can appear within hours of stopping drinking and range from mild anxiety to severe complications like seizures. Understanding these symptoms is crucial for effective treatment and recovery. This guide covers the causes, timeline, and treatment options to help you navigate through this challenging phase.
Key Takeaways
Alcohol Withdrawal Syndrome (AWS) entails a range of symptoms that can appear within 6 to 24 hours after ceasing alcohol intake, with severity classified into mild, moderate, and severe categories.
The pathophysiology of withdrawal involves a decrease in GABA activity and an increase in glutamate excitability, leading to overactivity of the central nervous system.
Effective treatment of alcohol withdrawal requires comprehensive medical intervention, including detoxification, medication management, and continuous supportive care to mitigate the risk of severe complications such as delirium tremens and withdrawal seizures.
Table of Contents
Recognizing Alcohol Withdrawal Symptoms

When a person significantly cuts down or discontinues their consumption of alcohol, they may begin to exhibit symptoms associated with Alcohol Withdrawal Syndrome (AWS), which can present within six to twenty-four hours following the last drink. The intensity and duration of these withdrawal symptoms are unpredictable, making it challenging to determine who will suffer from alcohol withdrawal and the severity of their experience. Prompt identification of such symptoms is crucial for successful treatment.
Withdrawal from alcohol usually manifests in three levels: mild, moderate, and severe. Mild cases might involve tremors, anxiety or irritability whereas someone experiencing mild withdrawal symptoms could also feel unsteady moderation conditions often include confusion and raised blood pressure intense scenarios may bring about hallucinations or seizures – this degree is potentially fatal if not medically addressed swiftly Recognizing these stages helps gauge how far along an individual’s withdrawal syndrome has progressed enabling timely medical response.
Early Symptoms
Symptoms of withdrawal from alcohol can emerge between six to twelve hours following the last consumption of alcohol. At this early phase, individuals might encounter manageable yet bothersome symptoms including headaches, feelings of anxiety, and sleep disturbances. These mild symptoms act as preliminary signals that the body is adjusting to not having alcohol in its system.
It’s crucial to recognize and respond to these initial signs without delay. Experiencing issues such as slight nervousness and difficulty sleeping may not appear critical, but they have the potential to worsen if left unattended. Early identification allows for prompt intervention which helps mitigate symptoms and averts more serious health complications related to withdrawal from alcohol.
Moderate Symptoms
During the progression of withdrawal, one may begin to experience more pronounced symptoms such as a rise in blood pressure, profuse sweating, and disorientation. These signs suggest considerable physiological adjustment in response to the lack of alcohol within the system. Careful observation is essential at this juncture to prevent these moderate indications from intensifying into severe or complicated withdrawal.
Symptoms like heightened blood pressure and heavy perspiration represent a step up from initial mild symptoms during alcohol abstinence and pose greater health risks. At this point, managed medical intervention can adeptly control these manifestations ensuring that individuals undergoing withdrawal do so with their safety maintained.
Severe Symptoms
The withdrawal from alcohol can lead to intense and potentially fatal symptoms. Hallucinations, seizures, and the particularly dangerous condition of delirium are among these severe manifestations. Delirium tremens stands out for its serious disturbances in autonomic functions coupled with hallucinatory experiences and demands urgent medical attention to avert deadly consequences.
Alongside physical effects, profound psychological distress including panic attacks and hallucinations may occur during alcohol withdrawal. To ensure safety, such symptoms often necessitate advanced medical management. The likelihood of experiencing these acute complications is heightened by factors like excessive alcohol consumption history and personal health issues—underscoring the critical importance of seeking expert care when withdrawing from alcohol.
Causes of Alcohol Withdrawal

Prolonged alcohol consumption leads to alterations in brain function, which is the underlying cause of alcohol withdrawal. Being a depressant that affects the central nervous system, alcohol slows down brain activity. If there’s a sudden decrease or cessation in drinking, it can cause an overstimulation of the central nervous system as it tries to adjust without the influence of alcohol. This results in withdrawal symptoms.
Factors such as personal body chemistry, how much and how often one drinks alcohol, along with other existing health issues, play roles in determining both intensity and length of these symptoms during withdrawal. Understanding these contributing factors helps explain why experiences with withdrawing from alcohol are complex and support personalized treatment protocols for those affected by them.
Role of GABA and Glutamate
Gamma aminobutyric acid (GABA) and glutamate, critical neurotransmitters, are deeply involved in the onset of symptoms associated with alcohol withdrawal. Prolonged alcohol use leads to diminished GABA receptor sensitivity, which plays an integral role in inhibitory signals within the brain. The suppressed activity of these receptors is partly why increased excitability occurs during the period of withdrawal.
In conjunction with this decreased activity in GABA receptors, chronic consumption of alcohol also causes an elevation in glutamate receptor levels—amplifying excitatory neurocommunication. This disparity between weakened GABA functioning and heightened glutamate action results in an over-stimulated state for the central nervous system when undergoing withdrawal from alcohol. Such complex biochemical dynamics underscore the challenges faced while trying to manage symptoms arising from discontinuation or reduction of alcohol intake.
Impact of Chronic Alcohol Use
Continuous use of alcohol can majorly change the brain’s chemical balance, making individuals more prone to experience intense withdrawal symptoms when they stop drinking. These altered neurological conditions also raise the potential for serious complications during withdrawal. For example, those with past incidents of stopping alcohol are at a higher risk for experiencing withdrawal seizures.
Extended intake of alcohol doesn’t just alter brain function. It also heightens the likelihood of developing grave health issues including problems related to excessive consumption like liver disease and diseases affecting heart and blood vessels.
Understanding how long-term use of alcohol affects an individual underscores the importance of thorough care and assistance throughout the process of withdrawing from it.
Stages of Alcohol Withdrawal
The process of alcohol withdrawal is categorized into three key stages: the Initial Stage, Peak Stage, and Late Stage. Recognizing each stage is crucial for effectively handling symptoms and securing a secure path to recovery. Distinctive symptoms and hazards are associated with each phase, and individual experiences can differ significantly.
Being aware of how these stages unfold over time aids in anticipating potential symptoms and accessing medical help when necessary. For instance, delirium tremens usually manifests between one to four days following the onset of alcohol withdrawal, underscoring why it’s important to keep a close watch on symptom development during this critical timeframe.
Initial Stage (6-12 Hours)
Within a timeframe of six to twelve hours following the consumption of the last alcoholic beverage, the first phase of alcohol withdrawal commences. During this period, prevalent symptoms such as tremors, anxiety, and difficulty sleeping emerge as signs that the body is beginning to respond to its lack of alcohol. These can cause considerable discomfort if not appropriately addressed.
Intervening promptly at this juncture is crucial for alleviating symptom intensity and averting Escalation into more acute stages of withdrawal. Managing early manifestations like elevated heart rate and perspiration can significantly facilitate easing through the withdrawal experience.
Peak Stage (24-72 Hours)
During the 24 to 72 hours after ceasing alcohol intake, individuals reach the climax of alcohol withdrawal, a pivotal period characterized by an escalation in withdrawal symptoms’ severity. This span is crucial for those undergoing these effects since it includes potential hazards such as seizures, especially prevalent within the initial two days after the last drink. The Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar), is frequently utilized during this phase to evaluate symptom intensity and inform treatment strategies.
At this juncture when symptoms are at their zenith, medical oversight becomes imperative to navigate associated risks and maintain patient safety. It accentuates the importance of adequate medical care in handling severe manifestations of alcohol withdrawal.
Late Stage (3-7 Days)
The final phase of alcohol withdrawal typically spans three to seven days, yet certain symptoms may endure for weeks or months. In this stage, individuals might struggle with ongoing issues like sleep disturbances and fluctuations in their mood. Despite being less severe than the peak symptoms, these residual effects can still significantly disrupt everyday activities and the overall healing process.
It is crucial to maintain medical care and support throughout this late stage to secure a complete recovery while managing any lingering symptoms. Recognizing that some symptoms have an extended duration underscores the importance of sustained therapy and assistance during recuperation from alcohol withdrawal.
Diagnosis and Assessment of Alcohol Withdrawal

The diagnosis of alcohol withdrawal syndrome requires a comprehensive review of the patient’s medical history and an extensive physical assessment. It starts with evaluating their drinking habits, specifically how much and how long they have been consuming alcohol. This information is essential for healthcare professionals to assess the risk and expected intensity of withdrawal symptoms.
A detailed physical examination is vital to gauge the extent of withdrawal symptoms while also identifying any concurrent health or mental issues that could affect the process of withdrawing from alcohol. Utilizing recommended screening tools for assessing disorders related to alcohol use such as AUDIT (Alcohol Use Disorders Identification Test) and CAGE questionnaires in conjunction with laboratory blood tests can offer a complete picture of the individual’s health status concerning their use of alcohol.
Clinical Evaluation
An in-depth clinical assessment is crucial for the precise diagnosis of alcohol withdrawal and deciding on the correct course of action. Such an evaluation should meticulously review patient history, concentrating particularly on how frequently and how much alcohol has been consumed. It’s also vital to detect any existing medical or psychiatric issues that might affect how withdrawal symptoms are managed.
Conducting a physical examination aids healthcare professionals in gauging the intensity of withdrawal symptoms, which enables them to customize treatments according to each person’s specific requirements. The swift recognition of signs related to alcohol withdrawal through careful clinical evaluations can significantly improve both treatment efficacy and recovery success rates.
CIWA-Ar Scale
The Clinical Institute Withdrawal Assessment for Alcohol, commonly referred to as the CIWA-Ar scale, is crucial in gauging the intensity of withdrawal symptoms experienced during alcohol withdrawal. It evaluates a range of indicators such as tremors, nausea, perspiration, anxiety levels and sensory disruptions to give an all-encompassing picture of an individual’s state.
Consistently applying the CIWA-Ar scale at hourly intervals when administering medication provides medical professionals with pertinent data that assists them in tailoring treatment strategies according to changes in the patient’s presentation. Continuous monitoring is essential for controlling severe symptoms and averting potential adverse outcomes associated with alcohol withdrawal.
Treatment Options for Alcohol Withdrawal
To successfully manage alcohol withdrawal, it’s important to engage in a medically supervised detoxification process, utilize appropriate medications, and receive supportive care. These elements are vital for a secure and effective recovery journey. It is of paramount importance for individuals with significant dependence on alcohol to collaborate with healthcare professionals in crafting a personalized detox strategy.
Collaboration with medical experts enhances the safety of the detoxification experience and boosts the likelihood of achieving successful management of alcohol withdrawal symptoms. Knowledge about various treatment alternatives and their advantages plays an essential role in effectively overcoming challenges associated with the withdrawal phase.
Medical Detoxification
Medical detoxification serves as a pivotal element in treating alcohol withdrawal, especially for those experiencing severe symptoms or susceptible to complications. The provision of inpatient care creates an environment where constant medical oversight and assistance is available. Such intensive care is crucial for controlling severe withdrawal symptoms and averting potentially fatal outcomes.
The utilization of medications within the context of inpatient detoxification aids significantly in the management of withdrawal symptoms from alcohol. The on-site availability of healthcare experts guarantees immediate intervention for any arising issues, thus enhancing the safety and regulation during the detox process.
Medications Used
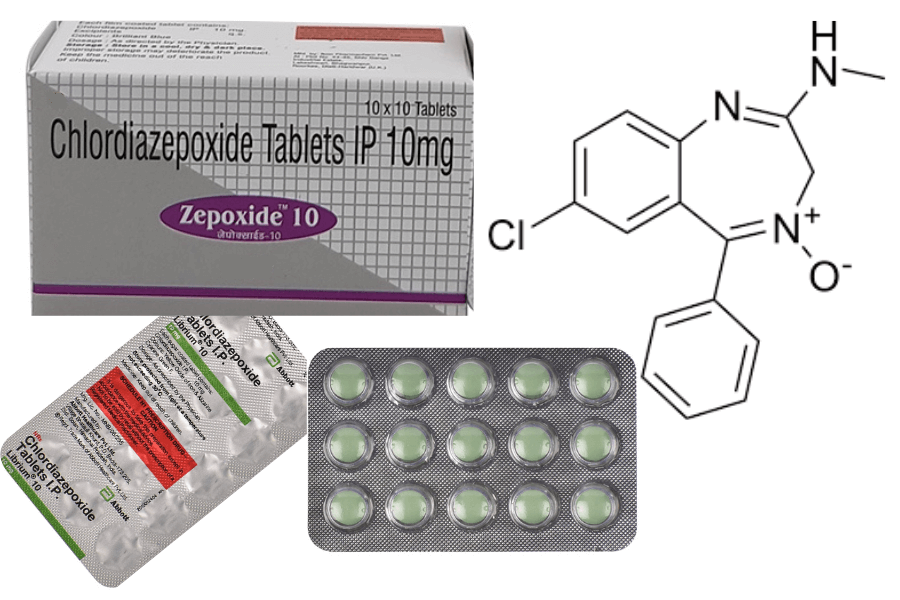
Pharmaceuticals are essential in controlling symptoms of alcohol withdrawal and thwarting grave complications. For mitigating the effects of withdrawal from alcohol and averting critical states including delirium, benzodiazepines stand out as the premier treatment option. To address mild to moderate withdrawal manifestations, other medications like carbamazepine may also be employed.
Employing alcohol in an attempt to manage its own withdrawal symptoms is ill-advised. With proper oversight from healthcare professionals for medication regulation, one can notably diminish the perils associated with severe withdrawals from alcohol and improve prospects for recuperation.
Supportive Care
Treating alcohol withdrawal effectively requires comprehensive supportive care, which emphasizes the importance of hydration and balanced nutrition. To mitigate symptoms and bolster health throughout recovery, it is crucial to address potential deficiencies in vitamins and minerals that individuals recovering from alcohol dependency might encounter.
The presence of a nurturing support system consisting of family members and friends is equally critical during the recovery journey. This network provides much-needed assistance in managing withdrawal symptoms while creating an optimistic environment that promotes recuperation.
Complications of Severe Alcohol Withdrawal
Experiencing severe symptoms of alcohol withdrawal, including delirium symptoms and autonomic instability, can escalate to life-threatening situations. Urgent medical care is imperative for those suffering from hallucinations or seizures as a result of withdrawing from alcohol. Immediate action should be taken by either visiting the nearest emergency room or contacting 911 if such symptoms manifest.
For individuals enduring severe alcohol withdrawal, management within an intensive care unit (ICU) is essential to provide them with secure conditions and appropriate medical attention. Acknowledging the gravity of these complications highlights the critical need for expert support throughout the withdrawal process.
Delirium Tremens
Delirium tremens presents with intense hallucinations and significant autonomic instability. It has been observed that women may exhibit a reduced number of autonomic symptoms when suffering from delirium tremens than their male counterparts. To control the symptoms and avoid any complications, treatment comprises medical oversight, pharmacological interventions, and supportive care.
Ensuring those afflicted by delirium symptoms receive adequate medical attention is crucial for appropriate management and timely intervention. Safeguarding patient well-being necessitates a strictly regulated environment to handle this condition effectively and securely.
Withdrawal Seizures
Severe symptoms can arise during alcohol withdrawal, withdrawal seizures being a significant concern. These seizures typically manifest 24 to 48 hours following the discontinuation of alcohol and signify an elevated level of danger that necessitates immediate medical attention for the prevention of additional issues and safeguarding patient well-being.
To effectively control these severe symptoms associated with alcohol cessation, medical personnel must administer appropriate medication and perform constant supervision. This approach is crucial in reducing the adverse health effects posed by alcohol withdrawal seizures on individuals undergoing treatment.
Preventing Alcohol Withdrawal Syndrome
A tactical method to diminish alcohol intake is essential in averting alcohol withdrawal syndrome. By incrementally lessening the consumption of alcohol, one’s body can acclimate, thereby mitigating the likelihood of experiencing withdrawal symptoms. A methodical scheme for scaling down on drinking could substantially decrease the chance of severe withdrawal.
The assistance and direction from healthcare experts are pivotal throughout this endeavor. They have the capacity to devise customized detoxification strategies that guarantee both safety and efficacy while managing withdrawal syndrome. Acknowledging the importance of a stepwise reduction in conjunction with professional aid is key to staving off intense symptoms associated with withdrawing from alcohol.
Gradual Reduction
A steady decrease in alcohol consumption can considerably lessen the dangers associated with withdrawal, thereby making it a more secure and controllable endeavor. Individuals aiming to manage withdrawal symptoms safely may find assistance through numerous treatment methodologies, which incorporate medication and medical oversight.
It is critical to seek advice from healthcare professionals who are equipped to devise detoxification strategies that cater specifically to personal requirements. By carefully tapering off alcohol intake, the body has an opportunity for gradual adjustment, diminishing the potential for severe withdrawal effects.
Professional Help
Seeking the guidance of healthcare experts can lead to customized detoxification strategies designed to safeguard individuals throughout their withdrawal journey. For those who may encounter severe symptoms or face potential complications, professional help is vital as it enables constant observation and immediate action when necessary.
Medical professionals are equipped to deliver specialized care and various treatment alternatives tailored to suit the unique requirements of each person, thereby increasing the chances of a secure and effective detox process.
Long-Term Recovery and Support
Continued backing is imperative for those recuperating from substance use afflictions to uphold abstinence and diminish the chances of a recurrence. Sustained support and treatment play an integral role in preserving sobriety following the initial phase of withdrawal.
The involvement of family plays a critical role in aiding recovery, providing both emotional support and tangible aid for individuals grappling with alcohol withdrawal. Incorporating relatives into therapeutic sessions can bolster the process by reinforcing networks of support while tackling issues within family dynamics.
Counseling and Therapy
Therapeutic interventions on both an individual and group level can greatly improve the journey to recovery, equipping individuals with coping mechanisms and offering much-needed emotional support. These therapeutic encounters are crucial in tackling the psychological elements involved in recuperating from alcohol use disorder.
On one hand, individual therapy delivers tailor-made guidance that delves into the root causes of addiction, promoting profound understanding and methods for managing it. On the other hand, group therapy provides a communal environment where shared experiences play an essential role in supporting ongoing abstinence from alcohol use.
Support Groups
Being a part of support groups, including Alcoholics Anonymous, plays a crucial role in bolstering accountability and providing collective backing during the recovery process. The communal connection and commonality found within these groups are essential elements for achieving sustained abstinence.
Such support circles as Alcoholics Anonymous amplify the advantages of expert treatment through social encouragement. Membership in these communities cultivates feelings of inclusion and assists members in remaining dedicated to their path toward recovery.
Family Involvement
Having a family that provides support is crucial during recovery, as they can offer both emotional comfort and tangible help for individuals undergoing alcohol withdrawal. The presence of a caring family atmosphere can alleviate the common feelings of tension and anxiety associated with withdrawal.
Involving family members in therapy sessions can be beneficial to identify and resolve any deep-seated problems present in the relationships among relatives which could potentially influence alcohol addiction. Family therapy ensures that all involved are on the same page regarding the path to recovery.
Summary
In essence, it is critical to comprehend the onset and progression of symptoms associated with alcohol withdrawal for its successful management and recovery. Early identification of initial, intermediate, and severe indicators can lead to prompt intervention that lowers potential complications. The involvement of GABA and glutamate underscores the intricate nature of biochemical reactions during this process.
To manage these symptoms effectively, approaches such as medical detoxification programs, pharmacological treatments, and supportive care are indispensable in ensuring a safe withdrawal experience. Taking steps like gradually reducing alcohol consumption under professional guidance can help avoid the onset of alcohol withdrawal syndrome while optimizing recovery results. A long-term strategy incorporating therapy sessions along with family support plays an important role in maintaining abstinence from alcohol and mitigating relapse risks.
Individuals on their journey towards overcoming addiction should leverage available resources by seeking expert assistance which facilitates managing challenges linked to withdrawing from alcohol—a path demanding perseverance, comprehensive support networks, and dedication toward achieving lasting sobriety.
Frequently Asked Questions
What are the early symptoms of alcohol withdrawal?
Symptoms of alcohol withdrawal Appear between six to twelve hours following consuming the last alcoholic beverage and can include sensations such as headaches, feelings of anxiety, and difficulty sleeping.
It is essential to identify these early indications promptly in order to obtain the necessary help and medical care.
How long do severe symptoms of alcohol withdrawal last?
Symptoms associated with severe alcohol withdrawal usually emerge within 24 to 72 hours following the consumption of the last drink and can require immediate medical attention.
It is imperative to seek expert help during this crucial time frame.
What role do GABA and glutamate play in alcohol withdrawal?
GABA and glutamate play critical roles in alcohol withdrawal, as chronic alcohol use reduces GABA receptor responsiveness while increasing glutamate receptor levels.
This imbalance results in intensified withdrawal symptoms when alcohol consumption is abruptly stopped.
How can alcohol withdrawal syndrome be prevented?
Preventing alcohol withdrawal syndrome can be effectively achieved by gradually reducing alcohol intake and seeking guidance from healthcare professionals for a personalized detoxification plan.
This approach minimizes the risk of severe withdrawal symptoms and promotes safer recovery.
What support options are available for long-term recovery from alcohol withdrawal?
Individual and group therapy, alongside engagement in support groups such as Alcoholics Anonymous and the inclusion of family members, are vital components for a successful long-term recovery from alcohol withdrawal.
Together, these elements contribute to a stronger pathway toward recovery.
Dr. Mitchell G. Cohen is a board-certified Internal Medicine specialist with over 34 years of experience in patient-centered healthcare. A graduate of Hahnemann University School of Medicine, Dr. Cohen completed his internship at the University Health Center of Pittsburgh, where he gained invaluable hands-on experience. He is also a certified addiction specialist, holding membership with the American Society of Addiction Medicine (ASAM).
Currently based in Nashua, NH, Dr. Cohen is affiliated with Saint Joseph Hospital, where he provides comprehensive care focusing on both internal medicine and addiction treatment. His expertise includes prevention, diagnosis, and management of adult diseases, as well as specialized care for individuals facing substance use disorders.
Dr. Cohen is committed to fostering open communication, ensuring his patients are fully informed and empowered to make confident decisions about their health and treatment options.

MD Mitchell Grant Cohen
Dr. Mitchell G. Cohen is a board-certified Internal Medicine specialist with over 34 years of experience in patient-centered healthcare. A graduate of Hahnemann University School of Medicine, Dr. Cohen completed his internship at the University Health Center of Pittsburgh, where he gained invaluable hands-on experience. He is also a certified addiction specialist, holding membership with the American Society of Addiction Medicine (ASAM).
Currently based in Nashua, NH, Dr. Cohen is affiliated with Saint Joseph Hospital, where he provides comprehensive care focusing on both internal medicine and addiction treatment. His expertise includes prevention, diagnosis, and management of adult diseases, as well as specialized care for individuals facing substance use disorders.
Dr. Cohen is committed to fostering open communication, ensuring his patients are fully informed and empowered to make confident decisions about their health and treatment options.
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen
- MD Mitchell Grant Cohen







